Picture this: you get up to grab yourself a cup of coffee, and by the time you reach the kitchen your heart is hammering like you just ran suicides in gym class. You’re dizzy. Vision grays out. You sit and you’re fine, so you stand up again, repeat. Doctors shrug. TikTok keeps calling it “random anxiety.” People keep asking you if you’re drinking enough water. Enough with the water question already!
It could actually be Postural Orthostatic Tachycardia Syndrome, better known by its nickname POTS, and it loves to coexist with ADHD, if only to make your life a little more complicated.
What POTS Is, Actually:
When you stand, gravity drags blood toward your legs. A well-tuned nervous system squeezes vessels and nudges heart rate just enough to keep blood and its oxygen reaching your brain, so you stay upright instead of blacking out.
With POTS the squeeze never kicks in. Blood pools in the legs, the heart races to compensate, but not enough blood makes it upstairs. Dizziness hits fast and you need to sit before you hit the floor.
POTS is not just dehydration or everyday anxiety. It is an autonomic wiring glitch that needs its own plan: extra salt, plenty of fluids, compression gear, and a doctor who knows the drill.
It shows up mostly in women, often starting in the teen or early-adult years, and can flare after illness, surgery, or a big growth spurt.
Heat, hot showers, long lines, skipped meals, dehydration, and period week can crank symptoms.
Diagnosis comes from a standing test or a tilt table test at a cardiology or autonomic clinic. It is more than a quick “drink more water” chat.
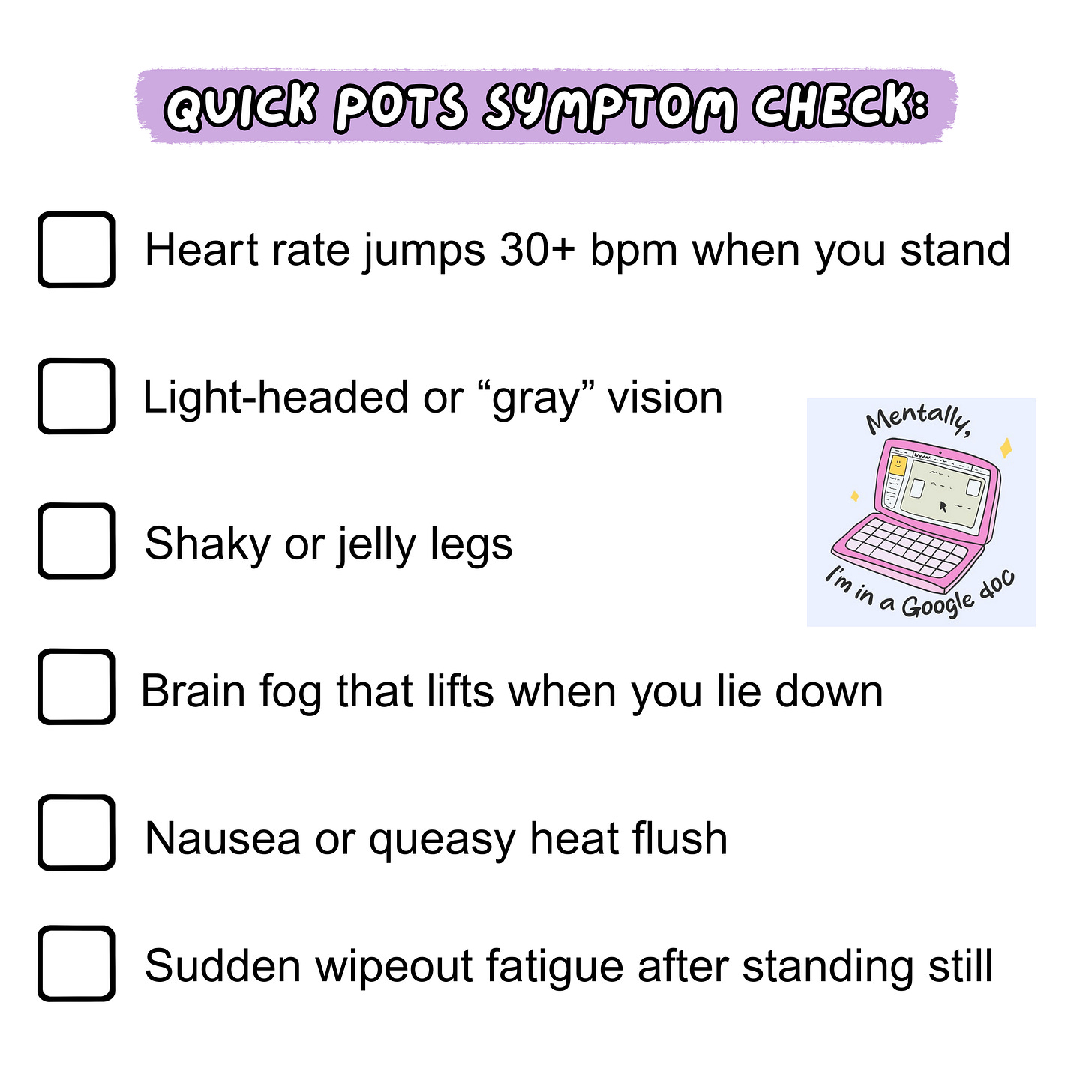
Quick home check. Take your pulse while lying down. Stand and check again after two minutes. A jump of roughly thirty beats per minute is a red flag to mention to your doctor.
ADHD + POTS, the Tag-Team Effect:
About 60% of people diagnosed with POTS also land in the ADHD range on focus tests. Six out of ten waiting-room chairs, give or take.
The overlap shows up two ways. Some people have lifelong ADHD that finally gets noticed once POTS sends them to a doctor. Others never had classic childhood symptoms, but the constant adrenaline spikes and low blood flow of POTS can mimic ADHD in adulthood. Either way the brain fog is real and needs help.
Low blood volume keeps the body stuck in light fight-or-flight. Adrenaline races the heart and floods the thinking part of the brain, so pulse and focus spin together.
ADHD traits then sabotage POTS care. You forget salt tablets, skip water, lose track of time standing in line, and trigger the next dizzy rush.
The loop can break. Steady the body with salt, fluids, compression, and a POTS-literate doctor. Steady the brain with clear cues, gentle structure, and meds that do not spike heart rate. Each side calms the other.
Quick POTS Questions (With an ADHD Lens):
Does plain water fix the dizziness?
Not by itself. Salt keeps the water in your bloodstream so pressure does not crash when you stand. ADHD brains often forget salt. Pair water with pre-measured salty snacks or tablets you can see and grab fast.
If I get my ADHD under control will POTS calm down?
Better focus helps you remember salt, water, and socks, which can shrink dizzy spells. It will not fix the blood-vessel glitch, so you still need the POTS care plan.
Can ADHD meds make POTS feel worse?
Stimulants raise heart rate for some people. Track your standing pulse for a week and bring the numbers to your prescriber so they can adjust dose or switch to a non-stimulant that plays nicer with your heart.
How do I remember all this when ADHD makes routine hard?
Use external cues. Phone alarms named “Salt Now,” bottles marked with time lines, or a sticky note on the kettle. Offload the remembering to objects and apps.
Do compression socks really matter?
Yes. Knee-high twenty-to-thirty millimeter socks push blood back up when vessels lag. Keep a pair by the door so ADHD inertia does not kill the habit.
Is exercise safe or will it make me faint?
Yes it is safe—when you stay seated at first. Rowing machines and recumbent bikes let your legs pump blood without you standing still. Short frequent sessions build leg strength and cut dizzy spells.
How We Close the Gap:
Most people get sliced-up advice.
A cardiologist says “salt and compression,” a therapist says “try mindfulness,” TikTok screams “just hydrate,” and none of it sticks because ADHD makes routine slippery while POTS punishes every slip. You leave each interaction with half a plan and a head full of static. That is why you leave each office with half a plan and zero relief.
Here’s how we fix that. You and me, baby, one on one. One session at a time.
You bring in the whole messy week with you.
Good moments. Flare ups. Bad moments. Random wins. Random randoms. Put everything on the table.
We spot the loops.
Behavioral, environmental, emotional. Maybe you skipped lunch, stood in a hot line, and forgot salt. The pieces click once we say them out loud.
You pick one tiny shift.
Add a salty snack to the lunch you already eat. Set a phone ping that says socks on now. Nothing huge. Something you can handle today.
You choose the cue that will actually reach you.
Calendar alert, sticky note on the coffee maker, electrolyte packets on your desk. The reminder has to live where you live.
Next session we check in.
What worked stays. What flopped turns into data, not failure, and we tweak the plan before old habits creep back.
Over time the basics run on autopilot.
Water, salt, compression, short seated workouts. Heart rate calms, focus sticks.
Then we tackle the rest of life.
With body drama quieter, the same method hits career moves, relationships, creative projects. You steer the conversation, not your symptoms.
Ready to break the loop? Grab a Deep Dive session here:
Not sure yet? Book a free 30-minute chat here:
This article is for education only and is not medical advice.